Whenever a tooth is removed from the bone and gums, blood coagulation protects the opening in your gums as it swells. If the blood coagulation doesn’t shape as expected or becomes expelled from your gums during recovery, it can result in a dry socket.
A dry socket is also called alveolar osteitis.
A dry socket can allow the nerves and bone in your gums to be exposed, so seeking dental care is critical. The situation can be unbelievably difficult, and whenever left untreated, it can prompt inconveniences, including:
- deferred mending
- infection in the socket
- infection that spreads deep down
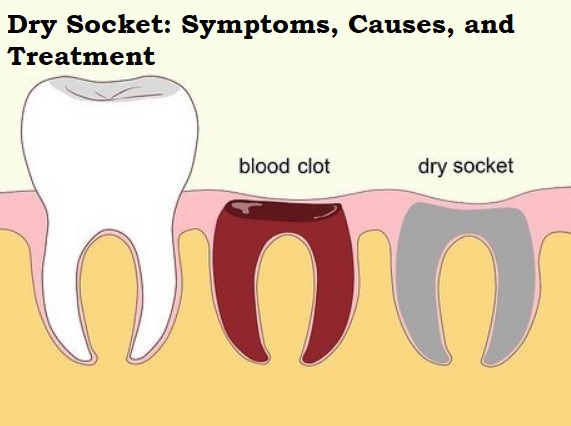
Table of Contents
Symptoms
Signs and side effects of dry socket might include:
- Extreme agony within a couple of days after a tooth extraction
- Halfway or complete loss of the blood coagulation at the tooth extraction site, which you might see as a vacant looking (dry) socket
- Noticeable bone in the socket
- The pain that transmits from the socket to your ear, eye, sanctuary, or neck on the same side of your face as the extraction
- Terrible breath or a foul smell coming from your mouth
- The terrible desire for your mouth
Who Is Likely to Get a Dry Socket?
It is possible for some people to develop a dry socket after having a tooth pulled. That incorporates individuals who:
- smoke
- have poor oral cleanliness
- pull wisdom teeth
- have a more prominent than-normal injury during the tooth extraction medical procedure
- use anti-conception medication pills
- have a past filled with dry sockets in the wake of having teeth pulled
- Flushing and spitting a lot or drinking through a straw after having a tooth extracted can also increase your risk of getting a dry socket.
How is a Dry Socket Analyzed?
Analysis of a dry socket depends on the historical backdrop of dental treatment, clinical assessment, and the patient’s side effects. The planning of when side effects start might be a sign of a dry socket. During basic repairs, the pain of extraction should reduce after some time. In any case, assuming the agony builds, this means that mending delays and might be because of a dry socket.
Normally, side effects of a dry socket appear two to four days after tooth extraction.
Most dry sockets occur within the first week after tooth extraction.
Causes
If a defensive blood cluster does not frame the open space after a tooth is extracted, a dry socket can develop.
A dry socket can also develop if this blood coagulation becomes expelled from your gums.
Analysts don’t know what prevents this blood coagulation from occurring. It’s believed that bacterial pollution, whether from food, fluid, or other things that enter the mouth, can cause dry sockets.
Injury to the area may also result in a dry socket. This can happen during complicated tooth extraction or aftercare. For instance, accidentally poking the area with your toothbrush might disturb the socket’s mending.
Treatment
Treatment for dry sockets aims to reduce pain. The American Dental Association recommends referring to a specialist right away to monitor side effects.
A dental specialist will clean the socket with cured mouthwash or saline. Then, at that point, they will fill in the socket with a sedated dressing to control the aggravation. Depending upon how long the pain lasts, patients might have to change this dressing after two or three days.
Grown-ups can also ingest nonsteroidal calming medications, like ibuprofen (Advil).
Recovery Time
Much of the time, the aggravation of dry socket works within 24-72 hours, as per the Canadian Dental Association. In some cases, the aggravation might last as long as 7 days.
However, a brief treatment can reduce the aggravation quickly. On the off chance that the socket dressing isn’t compelling, or the aggravation continues for longer than a couple of days, a dental specialist might reconsider checking whether another condition is liable for the aggravation.
Might you at any point have a dry socket with no aggravation?
For a great many people, the fundamental side effect of dry sockets is extreme pain. Be that as it may, coping with trauma varies from one individual to another. In this manner, certain individuals might encounter less torment than others.
Dental specialists will normally analyze dry sockets in light of the presence of pain and breakdown of the coagulation after tooth extraction.
The essential treatment for dry socket is tormenting the board, so assuming the condition causes practically zero torments, it doesn’t need treatment. The socket will swell up and get better by itself.
Nonetheless, getting a bacterial infection is a potential risk following a tooth extraction. Individuals with side effects that indicate a disease, like discharge from the socket, should seek treatment, regardless of whether the impacted area is not painful.
How Might I Prevent Dry Socket?
Since smoking is a major risk factor for dry sockets, stay away from cigarettes, stogies, and some other tobacco items for a day or so after your medical procedure. Assuming you take conception prevention pills, get some information about performing the extraction on a day when you are getting the most minimal amount of estrogen. Chemicals can influence the ability of the blood to cluster. Likewise, check with your dentist about different meds you are taking that can obstruct normal blood thickening.
After the procedure, refrain from drinking through a straw and spitting for the next few days. Likewise don’t wash your mouth more than your dentist suggests. If you do wash, do so delicately. Make an appointment with your dental specialist for all planned subsequent visits.
Risk factors
Factors that can increase your risk of creating a dry socket include:
Smoking and tobacco use. Synthetic substances in cigarettes or other types of tobacco might delay or slow healing and pollute the injury site. Sucking on a cigarette can help prevent blood clots.
Oral contraceptives. High estrogen levels from oral contraceptives might disturb normal mending cycles and increase the risk of dry socket.
Ill-advised at-home consideration. Inability to observe home-care rules and poor oral hygiene could increase the risk of dry sockets.
Having dry socket before. If you’ve had a dry socket previously, you’re bound to develop another extraction.
Tooth or gum disease. Current or past diseases around the separated tooth increase the risk of dry socket.
FAQs
The aggravation sometimes spreads to the ears, neck, and jaw. It can also be accompanied by shortness of breath. It’s anything but an infection and isn’t associated with swelling, redness, or fever. You usually can’t see a dry socket.
Generally speaking, the dry socket will go away on its own, but as it heals, the patient will probably continue to experience discomfort. Assuming that you in all actuality do decide to treat a dry socket at home, you want to clean the injury with cool water. You also want to inundate the socket with saline and keep a cloth over the socket.
Scientists by and large concur that bacterial disease doesn’t “cause” dry socket, so anti-microbials don’t assist with forestalling evaporate socket or speed the recuperating system except if there’s a functioning infection
To lessen your chances of dry socket, stay away from dry, crunchy, or chewy food varieties. These food varieties can reduce blood coagulation. All things being equal, pick delicate food sources like yogurt, fruit purée, eggs, and pasta.